Understanding the Intricate Relationship Between Lifestyle and Hormone Balance
Hormonal equilibrium is a cornerstone of human health, influencing metabolism, mood, reproductive function, and overall vitality. Recent expert analyses from San Diego’s leading endocrinologists and integrative medicine practitioners emphasize that lifestyle modifications can profoundly impact hormone regulation. This dynamic interplay challenges the reductionist view that hormone imbalances are resolvable only through pharmacological intervention, highlighting instead the synergistic potential of behavioral, nutritional, and environmental adjustments.
Advanced Lifestyle Interventions: Mechanisms and Clinical Applications
San Diego specialists underscore that targeted lifestyle changes—such as optimizing circadian rhythms, adopting nutrient-dense diets rich in phytoestrogens and omega-3 fatty acids, and implementing stress reduction techniques like mindfulness-based stress reduction (MBSR)—can modulate endocrine pathways at molecular and systemic levels. For example, consistent sleep hygiene enhances hypothalamic-pituitary-adrenal (HPA) axis stability, mitigating cortisol dysregulation, a common disruptor of sex hormone balance. Similarly, exercise regimens calibrated to individual metabolic profiles influence insulin sensitivity and leptin signaling, pivotal in maintaining hormonal homeostasis.
How Do Specific Dietary Patterns Influence Hormonal Feedback Loops?
Dietary patterns notably affect hormone biosynthesis and receptor sensitivity. San Diego experts advocate Mediterranean and plant-based diets, which provide antioxidants and bioactive compounds that attenuate inflammatory cytokines implicated in hormonal resistance states. The incorporation of adaptogenic herbs such as ashwagandha and maca, as detailed in natural hormone balance recommendations, further supports endocrine resilience by modulating stress hormone cascades.
The Role of Environmental and Behavioral Factors in Hormone Optimization
Experts from San Diego highlight that minimizing endocrine-disrupting chemical exposure—found in plastics, pesticides, and personal care products—and fostering behaviors that promote gut microbiome diversity are critical for hormone synthesis and metabolism. The gut-hormone axis, increasingly recognized for its complexity, suggests that probiotic and prebiotic interventions can indirectly enhance hormonal balance by regulating enterohepatic circulation of estrogens and androgens.
Integrating Lifestyle Strategies with Medical Hormone Therapies: A Synergistic Approach
While lifestyle change alone can significantly improve hormone profiles, many San Diego clinicians recommend combining these interventions with individualized bioidentical hormone replacement therapy (BHRT) for optimized outcomes. Understanding the nuances of such integrative protocols is essential, as outlined in the comprehensive guide to bioidentical hormone optimization, which details patient-specific considerations and monitoring strategies.
What Are the Challenges in Sustaining Long-Term Hormone Balance Through Lifestyle Alone?
Maintaining hormonal homeostasis solely through lifestyle adaptation presents challenges including individual genetic variability, environmental exposures, and psychosocial stressors that may necessitate adjunctive medical therapies. San Diego experts emphasize the importance of personalized plans that evolve with patient physiology and lifestyle changes, recommending regular endocrine evaluations to tailor interventions effectively.
For those interested in deepening their understanding of personalized hormone balancing strategies and contributing to the dialogue on advanced integrative approaches, we encourage visiting our contact page to connect with San Diego’s foremost hormone specialists.
According to a 2022 study published in The Journal of Clinical Endocrinology & Metabolism, lifestyle factors including diet quality, physical activity, and stress management play a significant role in modulating endocrine function and reducing the risk of hormone-related disorders (source).
Genetic and Epigenetic Influences on Hormone Regulation: The Frontier of Personalized Medicine
San Diego endocrinologists are increasingly recognizing that genetic predispositions and epigenetic modifications significantly influence individual hormone profiles and responses to lifestyle interventions. Polymorphisms in genes regulating estrogen metabolism, androgen receptor sensitivity, and enzymes like aromatase can modulate how patients respond to both natural and pharmacologic therapies. Epigenetic factors, influenced by environmental exposures and nutrition, further complicate hormone regulation by altering gene expression patterns without changing DNA sequences. This understanding underscores the necessity for personalized hormone optimization plans that integrate genomic data with lifestyle and medical therapies for enhanced efficacy and safety.
Cutting-Edge Behavioral Interventions: Neuroendocrine Modulation and Stress Resilience
Advanced behavioral therapies that target neuroendocrine pathways are gaining traction as adjuncts to conventional hormone therapies. Mindfulness-based interventions, cognitive-behavioral therapy (CBT), and biofeedback have demonstrated efficacy in modulating hypothalamic-pituitary-adrenal (HPA) axis activity, reducing cortisol levels and improving overall hormonal homeostasis. San Diego integrative clinics often combine these approaches with bioidentical hormone replacement therapy (BHRT) to amplify patient outcomes, particularly in managing menopausal symptoms and adrenal fatigue. More detailed insights on combining lifestyle with hormone therapies are available in our latest advances in natural hormone treatments.
Can Emerging Microbiome Therapies Revolutionize Hormone Balance Management?
The gut microbiome’s role in hormone regulation is a rapidly evolving area of research. Specific microbial communities influence the enterohepatic recycling of estrogens and androgens by producing enzymes like beta-glucuronidase, which can deconjugate hormones for reabsorption. Dysbiosis may lead to altered hormone levels contributing to conditions such as estrogen dominance or androgen deficiency. Probiotic and prebiotic interventions tailored to restore a balanced microbiome hold promise for non-pharmacologic hormone modulation, a frontier that San Diego specialists are cautiously optimistic about. For patients interested in exploring this, resources on long-term benefits of hormone balancing therapy provide valuable context.
Environmental Endocrine Disruptors: Navigating a Complex Landscape
Persistent exposure to endocrine-disrupting chemicals (EDCs) remains a formidable challenge for maintaining hormone balance. Compounds such as bisphenol A (BPA), phthalates, and certain pesticides mimic or antagonize natural hormones, potentially exacerbating imbalances. San Diego experts advocate rigorous reduction of EDC exposure through conscious choices in food packaging, personal care products, and household items. Additionally, detoxification protocols incorporating dietary antioxidants and liver-supportive nutrients may enhance clearance of these compounds, supporting endogenous hormone metabolism.
A 2023 review in Environmental Health Perspectives highlights the critical need for integrative strategies combining EDC exposure reduction with lifestyle and medical interventions to achieve sustainable hormonal health (source).
We invite readers to share their experiences or questions regarding advanced hormone balancing strategies in the comments below. Engaging in this dialogue not only enriches community knowledge but also supports personalized approaches to hormone health.
Precision Epigenetic Profiling: Tailoring Hormone Therapies at the Molecular Level
In the cutting-edge landscape of hormone optimization, San Diego’s leading clinicians are increasingly leveraging epigenetic profiling to customize therapeutic interventions. Unlike static genetic tests, epigenetic assessments capture dynamic modifications such as DNA methylation and histone acetylation patterns that influence gene expression related to hormone synthesis, receptor sensitivity, and metabolic clearance. For instance, hypermethylation of CYP19A1 promoter regions, which encode aromatase enzyme critical for estrogen biosynthesis, can attenuate estrogen production and manifest clinically as hormonal insufficiency despite normal gene sequences.
By integrating epigenetic biomarkers with traditional hormonal assays, practitioners can devise personalized lifestyle and pharmacologic protocols that precisely modulate gene expression pathways. Nutritional epigenomics, involving tailored intake of methyl donors like folate and choline, and histone deacetylase inhibitors from natural sources (e.g., sulforaphane in cruciferous vegetables), are being explored to recalibrate dysregulated hormone-related genes. This nuanced approach not only enhances treatment efficacy but also minimizes side effects by avoiding empirical dosing.
How Can Epigenetic Interventions Be Safely Integrated Into Hormone Optimization Regimens?
Safe implementation demands interdisciplinary collaboration between endocrinologists, geneticists, and nutrition experts. Patients undergo comprehensive molecular profiling, followed by phased introduction of epigenetic modulators alongside bioidentical hormone therapies. Continuous monitoring of epigenetic markers and hormone levels informs regimen adjustments, optimizing outcomes while preventing overcorrection. Ongoing clinical trials, such as those summarized in the Journal of Clinical Epigenetics, underscore the promise and complexity of this frontier.
For practitioners and patients interested in this transformative domain, consulting with San Diego’s integrative hormone specialists can provide access to cutting-edge diagnostics and individualized protocols.
Neuroendocrine Circuitry Modulation: Emerging Therapies for Stress-Induced Hormonal Dysregulation
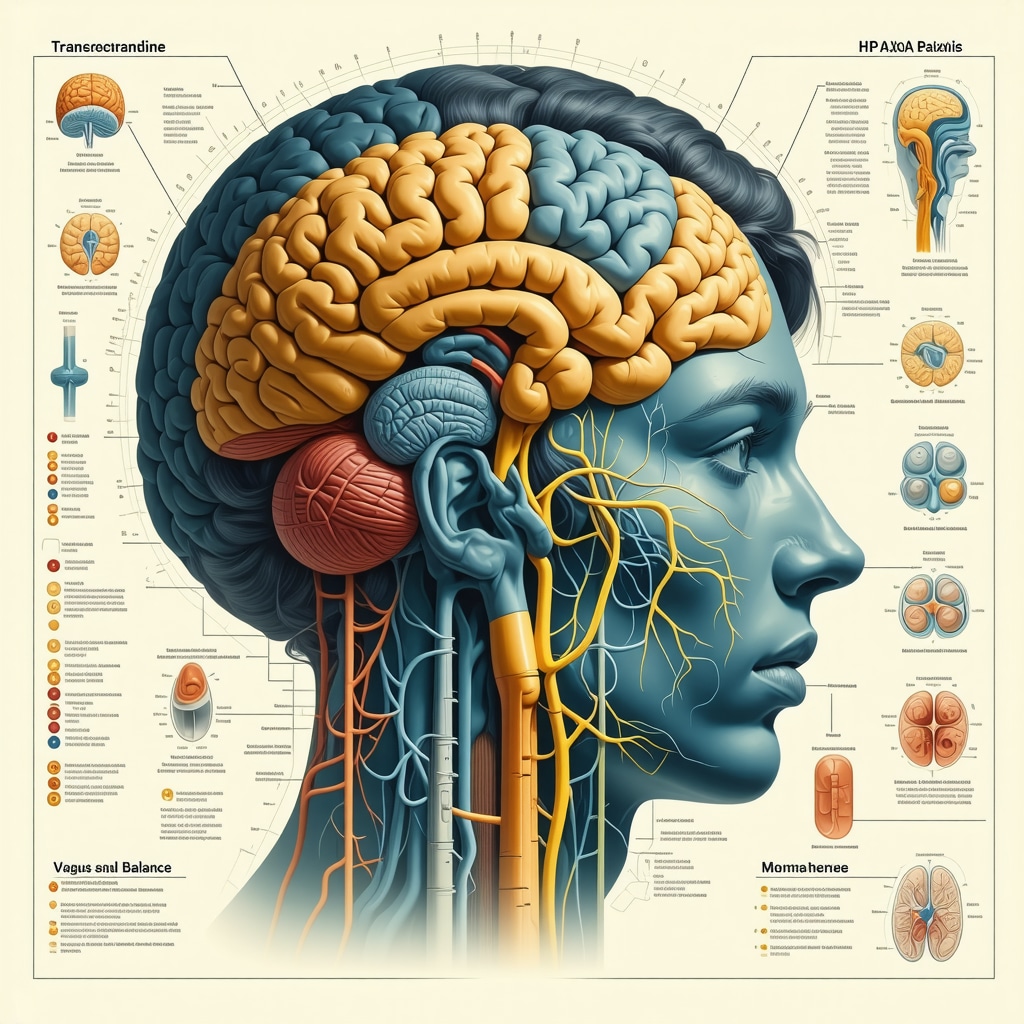
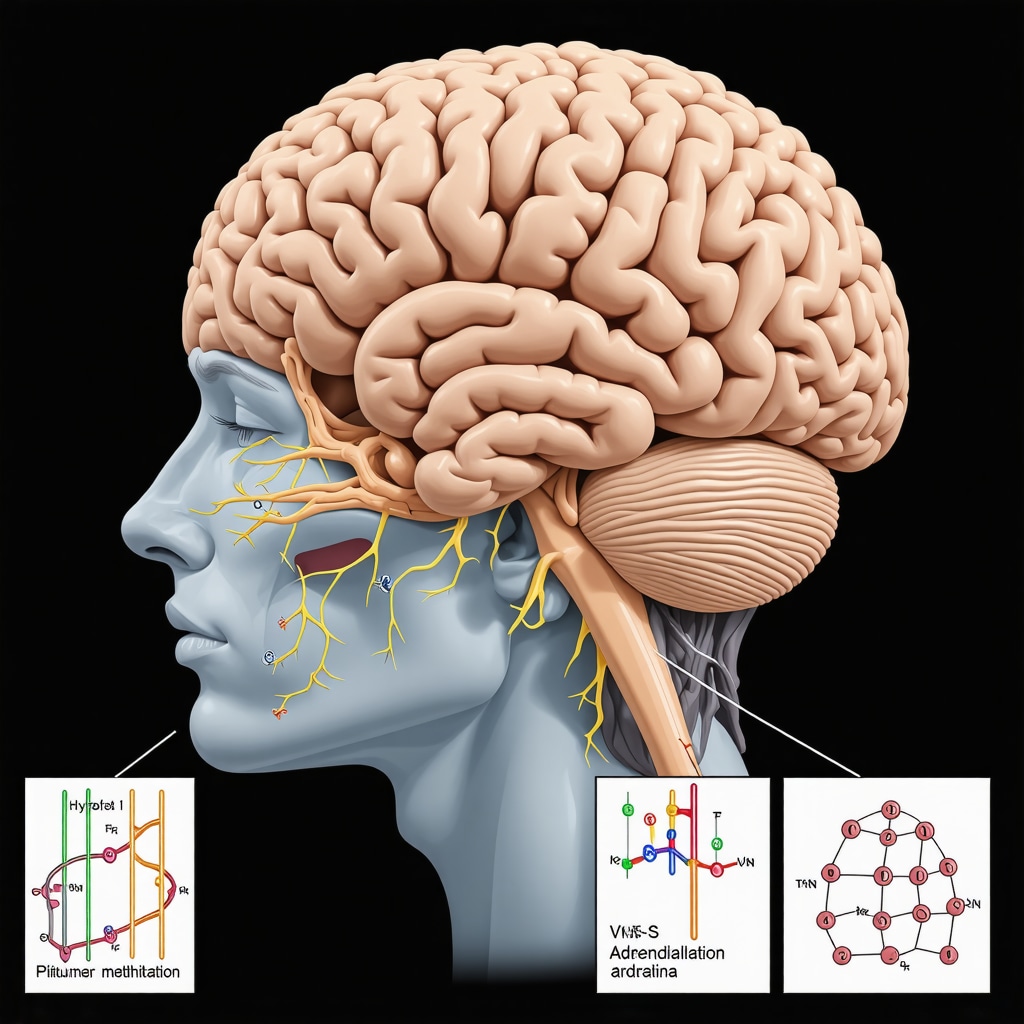
Beyond traditional stress reduction, recent innovations focus on direct modulation of neuroendocrine circuits governing hormonal axes. Techniques such as transcranial magnetic stimulation (TMS) and vagus nerve stimulation (VNS) are being investigated for their capacity to recalibrate HPA axis hyperactivity and restore hormonal homeostasis. Research from institutions like the National Institute of Mental Health demonstrates that targeted neuromodulation can reduce cortisol dysregulation, thereby improving sex hormone profiles and metabolic parameters.
Complementing these modalities, advanced biofeedback systems utilizing real-time hormonal and autonomic nervous system monitoring empower patients to gain conscious control over neuroendocrine responses. Such integrative protocols are particularly impactful for refractory cases of adrenal fatigue, perimenopause, and chronic stress syndromes.
What Are the Clinical Implications of Neuroendocrine Modulation in Hormone Therapy?
Clinical integration requires sophisticated assessment tools and interdisciplinary expertise to identify candidates who will benefit most. Early adopters report improved symptom control, reduced reliance on pharmacologic agents, and enhanced quality of life metrics. However, long-term data are still emerging, warranting cautious optimism and rigorous patient selection. San Diego clinics pioneering these therapies often combine them with personalized lifestyle adjustments and BHRT for synergistic effects.
Patients eager to explore these advanced neuroendocrine interventions should engage with experienced specialists to ensure safe, evidence-based application.
As this field evolves, continuous education and patient-centered research remain paramount. We encourage healthcare professionals and informed patients to delve deeper into these innovations by visiting our resource hub and joining expert-led webinars.
Epigenetic Remodeling: Precision Tools for Dynamic Hormonal Regulation
Building upon foundational genetic insights, San Diego endocrinologists are pioneering the integration of epigenetic remodeling to precisely recalibrate hormone pathways. This involves leveraging advances in molecular diagnostics to identify aberrant DNA methylation, histone modifications, and non-coding RNA influences that perturb endocrine function. Tailored interventions utilizing nutraceutical epigenetic modulators—such as folate, betaine, and sulforaphane—offer promising avenues to restore gene expression balance affecting aromatase activity, androgen receptor sensitivity, and glucocorticoid receptor function.
How can emerging epigenetic therapies be synergized with lifestyle modifications to enhance hormonal homeostasis?
Clinical protocols emphasize a phased, personalized approach where epigenetic therapies complement diet, stress management, and exercise regimens. For instance, methyl donor-rich diets enhance DNA methylation patterns conducive to balanced hormone synthesis, while mindfulness practices can mitigate stress-induced epigenetic disruptions of the HPA axis. Continuous biomarker monitoring ensures responsive adjustments to therapy, optimizing efficacy and minimizing adverse effects. Recent clinical trials, such as those detailed in the Journal of Clinical Epigenetics, provide evidence supporting this integrative methodology.
Neuroendocrine Circuit Modulation: Frontier Technologies and Clinical Translation
In tandem with molecular strategies, neuroendocrine modulation via neuromodulatory technologies is transforming approaches to stress-related hormonal imbalances. Techniques including transcranial magnetic stimulation (TMS) and vagus nerve stimulation (VNS) directly target dysregulated hypothalamic-pituitary-adrenal (HPA) axis circuits, attenuating maladaptive cortisol secretion patterns that disrupt sex hormone and metabolic homeostasis. These interventions, when integrated with biofeedback and cognitive therapies, empower patients to regain autonomic control over neuroendocrine responses, enhancing resilience to chronic stressors.
What are the practical considerations for incorporating neuromodulation into comprehensive hormone therapy programs?
Successful clinical adoption necessitates multidisciplinary evaluation to identify candidates exhibiting refractory HPA axis dysregulation. San Diego integrative clinics have reported significant symptom amelioration and decreased reliance on pharmacologic agents through combined neuromodulation and bioidentical hormone replacement therapy (BHRT). However, the heterogeneity of patient responses underscores the need for personalized treatment algorithms and ongoing research. The National Institute of Mental Health (NIMH) provides updated frameworks for ethical and effective neuromodulation deployment.
Synergistic Frameworks: Harmonizing Genomic, Epigenetic, and Neuroendocrine Therapies
Emerging evidence advocates for a comprehensive, integrative framework that harmonizes genomic profiling, epigenetic modulation, and neuroendocrine interventions. This multi-layered strategy enables clinicians to transcend traditional one-dimensional hormone therapies, tailoring regimens that dynamically respond to genetic predispositions, environmental exposures, and psychosocial stressors. Such sophistication demands advanced diagnostics, interdisciplinary collaboration, and patient engagement to optimize endocrine resilience and functional outcomes.
For clinicians and patients eager to delve into these advanced hormone optimization paradigms, we invite you to engage with San Diego’s foremost specialists through our contact page to explore personalized, cutting-edge protocols.
Expert Insights & Advanced Considerations
Integrative Approaches Amplify Hormone Stability Beyond Conventional Therapies
Leading San Diego endocrinologists emphasize that combining genomic, epigenetic, and neuroendocrine strategies with lifestyle modifications and bioidentical hormone replacement therapy (BHRT) creates a robust framework for sustained hormonal homeostasis. This synergy addresses multifactorial influences on endocrine function, enabling tailored interventions that transcend traditional one-size-fits-all protocols.
The Gut-Hormone Axis as a Critical Modulator in Hormonal Health
Emerging evidence highlights the gut microbiome’s enzymatic control over enterohepatic hormone recycling, which directly affects circulating estrogen and androgen levels. San Diego experts advocate for personalized probiotic and prebiotic regimens to restore microbial balance, thereby enhancing endogenous hormone metabolism and reducing reliance on pharmacologic agents.
Neuroendocrine Circuit Modulation Offers Promising Adjunctive Therapy
Advanced neuromodulation techniques such as transcranial magnetic stimulation (TMS) and vagus nerve stimulation (VNS) are gaining clinical traction for their ability to recalibrate hypothalamic-pituitary-adrenal (HPA) axis dysregulation. These modalities, integrated with BHRT and behavioral therapies, present a frontier in managing stress-induced hormonal imbalances and improving patient resilience.
Epigenetic Profiling Enables Dynamic and Precise Hormone Therapy Customization
Unlike static genetic data, epigenetic assessments reveal reversible modifications impacting hormone synthesis and receptor sensitivity. San Diego clinicians are pioneering protocols that incorporate nutritional epigenomics and targeted epigenetic modulators to fine-tune gene expression, optimizing both efficacy and safety in hormone balancing therapies.
Curated Expert Resources
The Journal of Clinical Endocrinology & Metabolism: A premier source for peer-reviewed studies on hormone regulation mechanisms and clinical interventions, essential for deepening understanding of lifestyle and pharmacologic impacts on endocrine health (source).
Journal of Clinical Epigenetics: Offers cutting-edge research on epigenetic influences in endocrine pathways, informing personalized hormone therapy strategies (source).
Environmental Health Perspectives: Provides comprehensive reviews on endocrine-disrupting chemicals (EDCs) and integrative approaches for minimizing their effects on hormonal balance (source).
National Institute of Mental Health (NIMH) Brain Stimulation Therapies: A valuable resource for understanding neuromodulation technologies applicable in hormone-related neuroendocrine disorders (source).
San Diego Hormone Therapy Resource Hub: For those seeking advanced clinical protocols and expert guidance on bioidentical hormone optimization, visit the comprehensive guide to bioidentical hormone optimization.
Final Expert Perspective
Contemporary hormone balancing therapy in San Diego is evolving into a sophisticated, multidimensional discipline that integrates genetic, epigenetic, microbial, and neuroendocrine insights with personalized lifestyle and hormonal interventions. The most impactful advances lie in this tailored synergy, enabling clinicians to optimize endocrine function with precision and responsiveness to individual variability. For healthcare professionals and patients committed to advancing hormone health, engaging with specialized experts and embracing these integrative strategies is paramount. To explore personalized, cutting-edge hormone balancing solutions, connect with San Diego’s leading specialists through our contact page and embark on a journey toward optimized vitality and hormonal well-being.

What really stood out to me in this discussion about lifestyle and hormone balance is the emphasis on the interconnectedness of our daily habits with endocrine health. I’ve personally noticed how disruptive poor sleep patterns can be—not just in feeling tired, but also in mood swings and cravings that could very well be tied to hormonal imbalances. The article’s explanation about how consistent sleep hygiene stabilizes the HPA axis makes a lot of sense given my experience. I’m curious, though, has anyone here experimented with combining behavioral changes, like mindfulness meditation or adaptive exercise routines, with targeted nutrition — for example, incorporating phytoestrogens or adaptogenic herbs like ashwagandha? It seems the San Diego experts are really onto the idea that a synergistic, personalized approach is necessary rather than relying simply on medications. Also, environmental factors like reducing exposure to endocrine-disrupting chemicals are often overlooked but must play a critical role. How do you navigate making these lifestyle changes manageable and sustainable amidst daily stress and busy schedules? Would love to hear others’ strategies for maintaining this holistic balance over time.