The Complex Physiology Behind Low Testosterone in Men Over 40
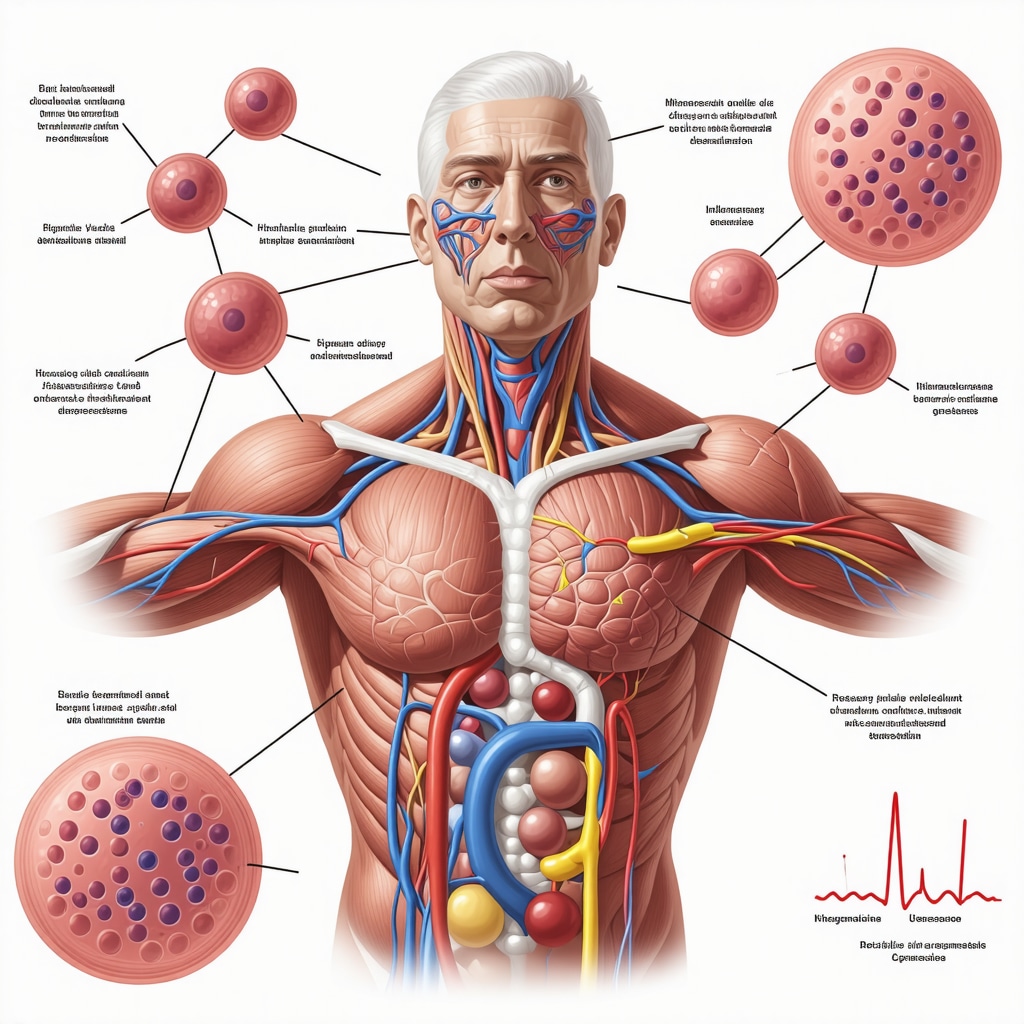
Testosterone decline after the age of 40 is a well-documented endocrinological phenomenon, yet its clinical manifestations and biochemical intricacies remain underappreciated outside specialist circles. This androgen, pivotal in regulating male secondary sexual characteristics, muscle mass, and metabolic functions, undergoes gradual attenuation influenced by multifactorial elements such as Leydig cell senescence, hypothalamic-pituitary axis alterations, and lifestyle-induced epigenetic modifications. In San Diego, where lifestyle and environmental factors interplay uniquely, understanding these endocrine shifts is crucial for effective diagnosis and management.
Advanced Clinical Indicators and Their Diagnostic Nuances
Recognition of low testosterone (hypogonadism) symptoms in men over 40 requires a nuanced approach encompassing both overt and subtle physiological signs. Classic symptoms include diminished libido, erectile dysfunction, decreased muscle strength, and increased adiposity. However, emerging evidence highlights cognitive impairments, mood disturbances, and metabolic syndrome components as integral clinical indicators. Biochemical evaluation must extend beyond total testosterone; assessing free testosterone and sex hormone-binding globulin (SHBG) levels provides a more precise hormonal milieu characterization, aligning with insights from endocrinology literature such as The Journal of Clinical Endocrinology & Metabolism.
How Do Lifestyle and Environmental Factors in San Diego Influence Low Testosterone Signs?
San Diego’s unique environmental exposures, including sun exposure impacting vitamin D synthesis and urban lifestyle stressors, modulate testosterone levels significantly. Sedentary habits, dietary patterns rich in processed foods, and cumulative stress contribute to hypothalamic-pituitary-adrenal (HPA) axis dysregulation, exacerbating hypogonadal symptoms. Integrating natural interventions such as tailored nutrition, exercise regimens, and stress management can synergistically enhance endogenous testosterone production. For a comprehensive approach to natural testosterone optimization, patients can explore San Diego’s best natural testosterone boosting strategies.
Integrating Bioidentical Hormone Replacement Therapy (BHRT) with Personalized Care
Bioidentical Hormone Replacement Therapy has gained traction as a precise modality to restore hormonal balance with molecular structures identical to endogenous hormones. In men over 40, BHRT offers symptom relief while minimizing adverse effects associated with synthetic analogs. Optimizing hormone pellet therapy, as detailed in San Diego’s hormone pellet therapy recovery timeline, requires careful patient-specific titration and monitoring to achieve physiological testosterone levels without provoking erythrocytosis or cardiovascular risk escalations. Collaboration with hormone specialists ensures tailored interventions aligned with individual metabolic and genetic profiles.
For men navigating the complexities of low testosterone, engaging with expert resources such as San Diego’s complete guide on low testosterone signs is invaluable for informed decision-making.
Expert-Level Strategies for Long-Term Hormonal Health Optimization
Beyond immediate symptom management, sustainable hormonal health demands an integrative strategy encompassing diet, exercise, sleep hygiene, and psychological well-being. Cutting-edge research underscores the role of combined BHRT and lifestyle modifications in mitigating age-related testosterone decline. San Diego-based protocols that fuse evidence-based medical therapies with holistic lifestyle adjustments, as highlighted in combining BHRT with diet and lifestyle, exemplify best practices for durable hormone balance and vitality restoration.
Explore further expert insights and contribute your professional experiences by visiting our community platform at Hormone Therapy San Diego contact page.
Emerging Biomarkers and Precision Diagnostics in Testosterone Optimization
While traditional assessments rely on serum testosterone levels, recent advances highlight novel biomarkers such as luteinizing hormone (LH), follicle-stimulating hormone (FSH), and adrenal androgens that refine hypogonadism diagnosis. These markers elucidate the axis dysfunction level—central or primary—and help tailor individualized therapies. Incorporating salivary and dried blood spot testing offers minimally invasive, dynamic monitoring options, enhancing patient compliance and therapeutic adjustments. This precision approach aligns with contemporary endocrinology paradigms aiming to optimize functional hormone balance rather than mere numeric targets.
Synergizing BHRT with Nutrigenomics and Lifestyle Interventions
Integrating bioidentical hormone replacement therapy with personalized nutrition based on nutrigenomic profiles represents a cutting-edge frontier. Genetic polymorphisms affecting hormone metabolism, receptor sensitivity, and inflammatory pathways modulate therapeutic responsiveness. For example, CYP450 enzyme variants influence testosterone clearance rates, necessitating dose customization. Lifestyle factors—such as circadian rhythm alignment, stress reduction techniques, and tailored physical activity—amplify BHRT benefits by stabilizing hormonal feedback mechanisms. Patients in San Diego can explore comprehensive programs combining these modalities through specialized clinics emphasizing holistic care, as detailed in combining BHRT with diet and lifestyle.
What Role Does Chronic Inflammation Play in Low Testosterone Among Men Over 40?
Chronic low-grade inflammation is increasingly recognized as a pivotal factor in age-related testosterone decline. Pro-inflammatory cytokines such as IL-6 and TNF-alpha disrupt hypothalamic signaling and reduce Leydig cell function, compounding hypogonadal symptoms. Addressing inflammatory burden through anti-inflammatory diets, omega-3 supplementation, and stress management improves endocrine function synergistically with hormone therapy. This inflammatory nexus underscores the necessity of comprehensive evaluation beyond hormone levels for efficacious management.
For clinicians and patients eager to delve deeper, Frontiers in Endocrinology’s review on inflammation and testosterone offers an authoritative synthesis of current evidence and therapeutic implications.
Advancing Patient Outcomes Through Integrative Hormone Pellet Therapy
Hormone pellet therapy, a minimally invasive BHRT delivery system, demonstrates consistent pharmacokinetics and superior patient adherence compared to conventional modalities. Understanding the recovery timeline and optimizing post-insertion care are paramount to maximizing clinical benefits while mitigating side effects, as explored in San Diego’s hormone pellet therapy recovery timeline. Multidisciplinary collaboration among endocrinologists, nutritionists, and mental health professionals fosters an integrative framework that addresses the multifactorial etiology of low testosterone.
Engage with our expert community by sharing your experiences or questions on hormone optimization at the Hormone Therapy San Diego contact page—your insights contribute to advancing personalized care.
Unraveling the Interplay Between Chronic Inflammation and Testosterone Decline: Molecular Pathways and Therapeutic Targets
Chronic low-grade inflammation emerges as a critical, yet often under-recognized, contributor to testosterone insufficiency in aging men. The persistent elevation of pro-inflammatory cytokines—namely interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP)—interferes with the hypothalamic-pituitary-gonadal (HPG) axis by disrupting gonadotropin-releasing hormone (GnRH) pulsatility and impairing Leydig cell steroidogenesis. This inflammatory milieu also induces oxidative stress, leading to mitochondrial dysfunction within Leydig cells, thereby compounding androgen biosynthesis deficits. Consequently, hypogonadism in this context is multifactorial, necessitating a holistic clinical approach that transcends mere serum testosterone quantification.
Emerging therapeutic strategies emphasize the integration of targeted anti-inflammatory interventions with hormone replacement protocols. Nutraceuticals rich in omega-3 fatty acids, curcumin, and flavonoids demonstrate immunomodulatory effects capable of attenuating cytokine overproduction, thereby potentially restoring HPG axis integrity. Moreover, lifestyle interventions encompassing Mediterranean-style diets, structured physical activity, and mindfulness-based stress reduction synergistically lower systemic inflammation, augmenting endogenous testosterone synthesis.
How Can Advanced Biomarker Panels Enhance the Precision of Testosterone Deficiency Diagnosis in Complex Cases?
Traditional reliance on total serum testosterone provides an incomplete picture, particularly in men with comorbidities such as obesity, metabolic syndrome, or chronic inflammatory states. Advanced biomarker panels that incorporate luteinizing hormone (LH), follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), adrenal androgen precursors like dehydroepiandrosterone sulfate (DHEA-S), and inflammatory markers (e.g., IL-6, TNF-α) allow clinicians to delineate the etiology of hypogonadism more precisely. For instance, elevated LH with low testosterone suggests primary testicular failure, whereas low or inappropriately normal LH indicates secondary hypogonadism involving hypothalamic or pituitary dysfunction.
Furthermore, integrating dynamic testing methods such as GnRH stimulation tests and serial hormone measurements via dried blood spots or salivary assays enhances temporal resolution and patient convenience. This multimodal diagnostic paradigm supports tailored treatment regimens, optimizing therapeutic efficacy while minimizing adverse effects. For a comprehensive review of these diagnostic advancements, consult the Clinical Endocrinology Journal’s article on precision diagnostics in male hypogonadism.
Synergistic Integration of BHRT with Nutrigenomics and Chronobiology: Pioneering Personalized Hormonal Care
Personalized medicine advances are revolutionizing testosterone therapy by incorporating genetic insights and circadian biology. Nutrigenomics examines individual genetic variations influencing nutrient metabolism and hormone regulation, facilitating bespoke dietary prescriptions that amplify BHRT outcomes. For example, polymorphisms in the CYP3A4 and CYP19A1 genes affect testosterone metabolism and aromatization rates, informing dosage and adjunctive strategies to mitigate estrogenic side effects.
Chronobiological considerations are equally pivotal. Testosterone exhibits diurnal variation, peaking in the early morning; thus, timing BHRT administration and lifestyle interventions to align with endogenous rhythms enhances hormonal homeostasis. San Diego clinics pioneering these approaches employ wearable technology to monitor circadian markers and customize treatment schedules accordingly.
Combining these modalities fosters robust hormonal equilibrium, improves patient quality of life, and mitigates long-term metabolic and cardiovascular risks. For detailed protocols integrating BHRT with nutrigenomics and chronotherapy, visit San Diego’s expert resource on BHRT and lifestyle synergy.
Emerging Therapeutic Frontiers: Peptide Modulators and Neuroendocrine Optimization in Male Hormonal Health
Innovative research is exploring peptide-based modulators such as kisspeptin and neurokinin B analogs that directly stimulate GnRH secretion, offering promising adjuncts for secondary hypogonadism. These neuroendocrine agents target upstream regulatory nodes, restoring physiological pulsatility and potentially enhancing endogenous testosterone production without exogenous hormone supplementation.
Clinical trials investigating the safety and efficacy of these peptides are underway, with preliminary data suggesting improvements in libido, mood, and metabolic parameters. Their integration with traditional BHRT may redefine therapeutic paradigms for men over 40 who exhibit complex neuroendocrine dysregulation.
To stay abreast of cutting-edge developments and personalized treatment options, healthcare professionals and patients are encouraged to engage with our expert community at the Hormone Therapy San Diego contact page.
Decoding the Molecular Interactions Linking Chronic Inflammation and Testosterone Deficiency
Recent advances elucidate how chronic low-grade inflammation mechanistically contributes to androgen decline through disruption of the hypothalamic-pituitary-gonadal (HPG) axis and mitochondrial impairment in Leydig cells. Pro-inflammatory cytokines — including IL-6, TNF-α, and CRP — interfere with gonadotropin-releasing hormone (GnRH) pulsatility, diminishing luteinizing hormone (LH) secretion and thus testosterone synthesis. Oxidative stress induced by this inflammatory milieu exacerbates mitochondrial dysfunction within testosterone-producing cells, highlighting a multifaceted pathophysiology that traditional serum testosterone measurements alone cannot capture.
How Can Advanced Biomarker Panels Enhance Diagnostic Precision in Complex Hypogonadism Cases?
For clinicians managing men over 40 with ambiguous symptomatic presentations and comorbidities such as metabolic syndrome or obesity, comprehensive biomarker profiling is indispensable. Panels encompassing LH, follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), adrenal androgen precursors like dehydroepiandrosterone sulfate (DHEA-S), alongside inflammatory markers (e.g., IL-6, TNF-α), enable a granular differentiation between primary and secondary hypogonadism. Integration of dynamic assessments such as GnRH stimulation tests, coupled with minimally invasive sampling techniques like salivary assays and dried blood spots, facilitates real-time hormonal monitoring and personalized treatment adjustments. For an in-depth discourse on these diagnostic innovations, refer to the Clinical Endocrinology Journal’s precision diagnostics review.
Synergistic Application of BHRT, Nutrigenomics, and Chronobiology in Personalized Testosterone Therapy
Emerging precision medicine paradigms advocate for the integration of bioidentical hormone replacement therapy (BHRT) with individualized nutrigenomic and chronobiological strategies. Genetic polymorphisms affecting enzymes such as CYP3A4 and CYP19A1 modulate testosterone metabolism and aromatization, necessitating personalized dosing regimens to optimize efficacy and minimize adverse effects. Furthermore, aligning BHRT administration with endogenous circadian rhythms, characterized by peak testosterone levels in early morning hours, potentiates hormonal homeostasis. Innovative San Diego clinics employ wearable biosensors to monitor circadian biomarkers, enabling dynamic therapy scheduling tailored to each patient’s biological clock.
This integrated approach not only enhances symptom amelioration but also reduces long-term cardiometabolic risks associated with hormonal imbalances. Explore comprehensive protocols for combining BHRT with lifestyle and dietary modifications at San Diego’s authoritative resource on BHRT and lifestyle synergy.
Exploring Peptide-Based Neuroendocrine Modulators: A New Horizon in Testosterone Restoration
Innovations in neuroendocrine therapeutics spotlight peptide modulators such as kisspeptin and neurokinin B analogs that act upstream to stimulate GnRH secretion, thereby restoring physiological pulsatility and enhancing endogenous testosterone production. These agents present promising adjunctive or alternative options for men with secondary hypogonadism refractory to conventional BHRT. Preliminary clinical trials demonstrate improvements in libido, mood stabilization, and metabolic profiles, indicating their potential to redefine management paradigms in male hormonal health.
Ongoing research endeavors continue to evaluate safety profiles and long-term efficacy, emphasizing the need for multidisciplinary collaboration to integrate these modalities effectively.
Engage with leading experts and stay informed on pioneering testosterone optimization strategies by visiting the Hormone Therapy San Diego contact page—advance your clinical practice or personal hormonal health journey.
Expert Insights & Advanced Considerations
Inflammation as a Central Modulator of Hypogonadism
Chronic low-grade inflammation profoundly disrupts the hypothalamic-pituitary-gonadal axis through cytokine-mediated impairment of gonadotropin-releasing hormone secretion and Leydig cell steroidogenesis. Addressing inflammatory pathways alongside hormone replacement is essential for comprehensive management of testosterone deficiency in men over 40.
Precision Diagnostics Beyond Total Testosterone
Utilizing advanced biomarker panels incorporating LH, FSH, SHBG, adrenal androgens, and inflammatory markers enhances diagnostic accuracy. Dynamic testing methods and minimally invasive collection techniques further enable personalized therapeutic strategies by delineating primary versus secondary hypogonadism etiologies.
Synergistic Integration of BHRT with Nutrigenomics and Chronobiology
Tailoring bioidentical hormone replacement therapy through genetic profiling and aligning treatment with circadian rhythms optimizes hormonal balance and mitigates side effects. This integrative approach leverages genetic polymorphisms affecting hormone metabolism and leverages chronotherapy for sustained endocrine homeostasis.
Emerging Neuroendocrine Peptide Modulators as Adjunctive Therapies
Innovative agents such as kisspeptin and neurokinin B analogs offer upstream stimulation of GnRH secretion, potentially restoring endogenous testosterone production in cases of secondary hypogonadism. These advances may complement traditional BHRT, expanding therapeutic options for complex cases.
Lifestyle Modifications Amplify Hormonal Therapy Outcomes
Comprehensive interventions including anti-inflammatory diets, targeted exercise, stress reduction, and optimized sleep hygiene significantly enhance BHRT efficacy and long-term hormonal health. The interplay between lifestyle and hormone therapy is critical in the holistic management of low testosterone.
Curated Expert Resources
- The Journal of Clinical Endocrinology & Metabolism: A premier source detailing the biochemical and clinical nuances of testosterone physiology and hypogonadism diagnostics.
- Clinical Endocrinology Journal’s Review on Precision Diagnostics: Offers an in-depth exploration of advanced biomarker panels and dynamic testing methodologies for male hypogonadism.
- Frontiers in Endocrinology’s Review on Inflammation and Testosterone: An authoritative synthesis on the molecular mechanisms linking chronic inflammation with androgen decline.
- San Diego’s Best Natural Testosterone Boosting Strategies: Practical guidance integrating lifestyle and environmental factors unique to the region for natural hormone optimization (link).
- Combining BHRT with Diet and Lifestyle: Comprehensive protocols demonstrating how personalized nutrition and lifestyle modifications augment bioidentical hormone therapy results (link).
Final Expert Perspective
Low testosterone in men over 40 is a multifaceted endocrinological challenge that demands a precision-based, integrative approach. Recognizing the pivotal role of chronic inflammation, leveraging advanced biomarker diagnostics, and personalizing BHRT through nutrigenomics and chronobiology are transforming therapeutic paradigms. Additionally, emerging neuroendocrine modulators promise to expand treatment horizons. Sustainable hormone health is best achieved by synergizing state-of-the-art medical interventions with targeted lifestyle strategies. Professionals and patients seeking to deepen their understanding or explore tailored solutions are encouraged to connect with specialized resources such as the Hormone Therapy San Diego contact page. This engagement fosters informed, collaborative pathways toward optimized hormonal vitality and well-being.

